Marcelina Głodowska: A Life Defined by Medical Challenges and the Fight for Development. Hyn
Marcelina Głodowska, known as Marcelinka, is a seven-year-old girl whose life has been defined by extraordinary medical challenges since before she was born. Her journey began in 2018, when her mother experienced a complicated pregnancy. Marcelinka was delivered at 33 weeks after her twin sister tragically passed at 21 weeks due to umbilical cord complications. While surviving the perinatal crisis, Marcelinka sustained significant health issues caused by interrupted oxygen supply, resulting in bilateral brain ischemia—a form of neonatal stroke that affected her entire neurological development.

Upon birth, Marcelinka was diagnosed with microcephaly, malformations of the frontal and parietal lobes, cranial dysmorphia (so-called “boat-shaped head”), and facial dysmorphism. Further neuroimaging confirmed polymicrogyria, a congenital defect of the cerebral cortex characterized by abnormal cortical folding. Polymicrogyria is extremely rare, occurring in roughly one in 100,000 live births, and it is often associated with severe motor, cognitive, and sensory impairments. For Marcelinka, this defect manifested as profound developmental delays, cerebral palsy affecting all four limbs, severe intellectual disability, hypertonicity, and epilepsy.
In addition to her neurological challenges, Marcelinka suffers from underdeveloped spinal discs, strabismus, and refractive errors that significantly compromise her vision. Her visual perception is limited; she recognizes familiar voices rather than faces, and responds primarily to auditory and tactile cues. Despite these severe limitations, Marcelinka shows moments of engagement, smiling or vocalizing when her condition allows. These small responses are critical markers of her interaction with the world and her ongoing developmental progress.


Marcelinka’s nervous system is highly sensitive, particularly to auditory stimuli, which can trigger heightened stress responses or seizure activity. Even minor changes in posture or routine can induce increased muscle tone, tremors, jaw clenching, and involuntary blinking, reflecting a Moro reflex that she cannot control. Her cerebral palsy prevents independent postural control; she cannot sit or stand without assistance. All repositioning must be carefully managed by caregivers, and she receives all nutrition through a PEG feeding tube due to her inability to safely swallow.
Given the complexity of her condition, Marcelinka has been under continuous specialized medical supervision since birth. Her care involves comprehensive neurodevelopmental monitoring, physical therapy, speech therapy, and occupational therapy tailored to her unique needs. In addition, she benefits from the oversight of a multidisciplinary team, including pediatric neurologists, neurosurgeons, ophthalmologists, cardiologists, gastroenterologists, and orthopedic specialists. Her ongoing education occurs within a specialized early childhood program designed for children with significant medical and developmental challenges, where curricula are individualized to support cognitive, sensory, and motor development.

The impact of Marcelinka’s medical conditions extends beyond the obvious physical limitations. The severity of her cerebral palsy and neurological deficits requires constant vigilance and intervention to prevent complications such as contractures, skin breakdown, and respiratory difficulties. Her hypertonia and limited mobility create a continuous risk for musculoskeletal deformities, necessitating careful positioning, physiotherapy, and adaptive equipment to promote skeletal and muscular health.
Marcelinka’s epilepsy, secondary to her cortical malformations, is persistent and severe. Seizures can be triggered by stress, fatigue, or sensory overload, and they frequently require rapid medical intervention to prevent prolonged episodes. Medication management is carefully titrated to balance seizure control with the potential for side effects, including sedation and gastrointestinal disturbances. Her condition necessitates constant observation, with caregivers trained to recognize subtle seizure activity and respond promptly.

Her cerebral palsy manifests as spastic quadriplegia, which severely limits voluntary movement and coordination. Physical therapy focuses on maintaining joint mobility, reducing spasticity, and improving functional positioning. Therapeutic exercises are performed multiple times daily to counteract the effects of hypertonia and prevent further musculoskeletal complications. Occupational therapy emphasizes fine motor development and adaptive techniques for daily care and interaction with her environment.
Marcelinka’s visual impairment presents additional challenges. Strabismus and uncorrectable refractive errors significantly reduce her visual acuity, limiting her ability to interact with her surroundings. Vision therapy is incorporated to stimulate visual processing, but her primary mode of environmental recognition remains auditory and tactile. Specialists continue to monitor her ocular health to prevent further deterioration and optimize her remaining vision.

Her feeding difficulties are managed through a PEG tube, providing consistent and safe nutrition. Oral intake is extremely limited due to impaired swallowing and the risk of aspiration. Nutritional support is essential to maintain growth, support immune function, and enable participation in rehabilitation therapies. Gastroenterologists oversee her feeding regimen, monitor for gastrointestinal complications, and ensure proper supplementation to prevent deficiencies.
Marcelinka’s condition also affects her respiratory function. Hypertonicity and limited mobility contribute to decreased pulmonary capacity, increasing her susceptibility to infections such as pneumonia. Pulmonology specialists collaborate with her care team to monitor lung function, provide respiratory therapy, and intervene rapidly in the case of infection or compromised breathing.

Her daily life is structured around the prevention of secondary complications and the promotion of developmental gains. Physical therapists, speech-language pathologists, and occupational therapists coordinate their interventions to provide a consistent, holistic approach. Therapy focuses on maintaining joint flexibility, stimulating cognitive and sensory pathways, promoting communication, and optimizing her functional abilities within her physical limitations.
The neurological complexity of her condition requires continuous reassessment. MRI scans and other neuroimaging modalities are periodically performed to monitor brain development, detect complications, and guide therapeutic interventions. Her care plan is dynamic, adapting to her evolving medical needs and developmental milestones.
Despite the profound severity of her impairments, Marcelinka demonstrates responsiveness to her environment. She recognizes familiar voices, smiles, and occasionally vocalizes, indicating social engagement and emotional awareness. These responses are nurtured through structured therapy, sensory stimulation, and attentive caregiving, forming the foundation for ongoing developmental progress.
Her spasticity and motor impairment necessitate specialized equipment to support posture and mobility. Adaptive seating, standing frames, and other assistive devices are critical to maintain skeletal alignment, prevent contractures, and provide opportunities for functional interaction with her environment. These devices are integrated into therapy sessions and daily care routines to maximize her physical potential.
Marcelinka’s care is a multidisciplinary effort requiring close coordination among medical professionals, therapists, and family members. Neurologists manage seizures and overall neurological health, neurosurgeons address structural brain concerns, ophthalmologists oversee her visual function, and cardiologists monitor cardiac health. Physical and occupational therapists implement individualized programs to promote movement, function, and comfort. Speech-language pathologists support communication and oral-motor development, while dietitians ensure adequate nutrition. Psychologists and educational specialists provide cognitive and emotional support.
Her long-term prognosis is guarded but focused on optimizing functional abilities, preventing complications, and maximizing quality of life. Continuous therapy, careful monitoring, and expert medical intervention aim to reduce the impact of her cerebral palsy, epilepsy, and visual impairment. Early intervention, consistency, and specialized care are critical to maintaining her progress and minimizing regression.

Marcelinka’s family plays a central role in her care. Every aspect of her daily routine—positioning, feeding, therapy exercises, and monitoring for seizures—relies on their vigilance and dedication. This constant engagement supports her development and ensures timely response to medical needs, forming a critical component of her overall care strategy.
The challenges Marcelinka faces are both medical and developmental. Her condition affects motor skills, cognitive function, communication, vision, and social interaction. Addressing these interrelated issues requires a holistic approach, integrating medical treatment, rehabilitative therapy, and environmental adaptations. Each day is carefully structured to balance therapeutic intervention, rest, nutrition, and emotional support.
In addition to the physical and neurological challenges, Marcelinka’s condition necessitates ongoing assessment of growth, bone health, and organ function. Multisystem involvement is common in children with severe cerebral palsy and congenital brain malformations, and proactive monitoring is essential to prevent complications and maintain stability.
Marcelinka’s epilepsy remains a central concern. Seizures can be prolonged and unpredictable, requiring rapid response and precise medication management. Her treatment regimen is carefully coordinated among neurologists, therapists, and caregivers to optimize seizure control while minimizing side effects.
Her cerebral palsy, visual impairment, and feeding difficulties intersect, creating complex challenges for everyday care. Physical therapy, occupational therapy, and adaptive strategies work synergistically to enhance her abilities, prevent secondary complications, and support functional independence as much as possible.
Despite the severity of her medical conditions, Marcelinka continues to demonstrate resilience and responsiveness. With appropriate support, ongoing therapy, and vigilant medical care, she continues to make incremental progress in motor function, sensory processing, and social engagement.
Marcelinka’s journey exemplifies the profound impact of congenital brain malformations, cerebral palsy, and multisystem developmental challenges. Her ongoing care illustrates the importance of multidisciplinary intervention, early and continuous therapy, and coordinated medical oversight to optimize outcomes and maintain quality of life.
While her condition is chronic and severe, Marcelinka continues to interact with her environment, respond to stimuli, and benefit from intensive therapies. Each day represents a careful balance of medical management, developmental stimulation, and family support, aimed at fostering her abilities and maintaining her health.
Her story highlights the complexity of managing severe congenital neurological and musculoskeletal disorders in children. It demonstrates how integrated care—combining medical intervention, rehabilitation, and family support—can sustain development, reduce complications, and enhance quality of life for children facing profound challenges.
Marcelinka’s life, while defined by medical adversity, is also characterized by small triumphs: responses to familiar voices, smiles during therapy, and moments of engagement that reflect her ongoing development. Each response underscores the significance of comprehensive care and the potential for progress, even in the context of profound disability.
In summary, Marcelinka Głodowska’s condition involves multiple congenital and acquired impairments: polymicrogyria, cerebral palsy, severe intellectual disability, epilepsy, hypertonia, visual impairment, and dysphagia requiring PEG feeding. Her care is continuous, intensive, and multidisciplinary, involving neurology, neurosurgery, cardiology, ophthalmology, gastroenterology, orthopedics, therapy services, and specialized early childhood education. Her prognosis focuses on maintaining health, maximizing developmental potential, and providing the highest achievable quality of life within the constraints of her complex medical condition.
Marcelinka’s story illustrates the ongoing challenges faced by children with severe congenital neurological and musculoskeletal disorders. It highlights the importance of comprehensive, multidisciplinary care, attentive rehabilitation, and constant monitoring to address the physical, cognitive, and sensory complications inherent in such conditions.
Even with profound limitations, Marcelinka continues to respond to her environment, demonstrating moments of engagement, emotion, and awareness. Her life exemplifies the intersection of medical complexity, developmental care, and family dedication, emphasizing the importance of holistic approaches in the treatment of children with severe disabilities.
Oscar – The Cat Who Could Sense the Final Moments of Life
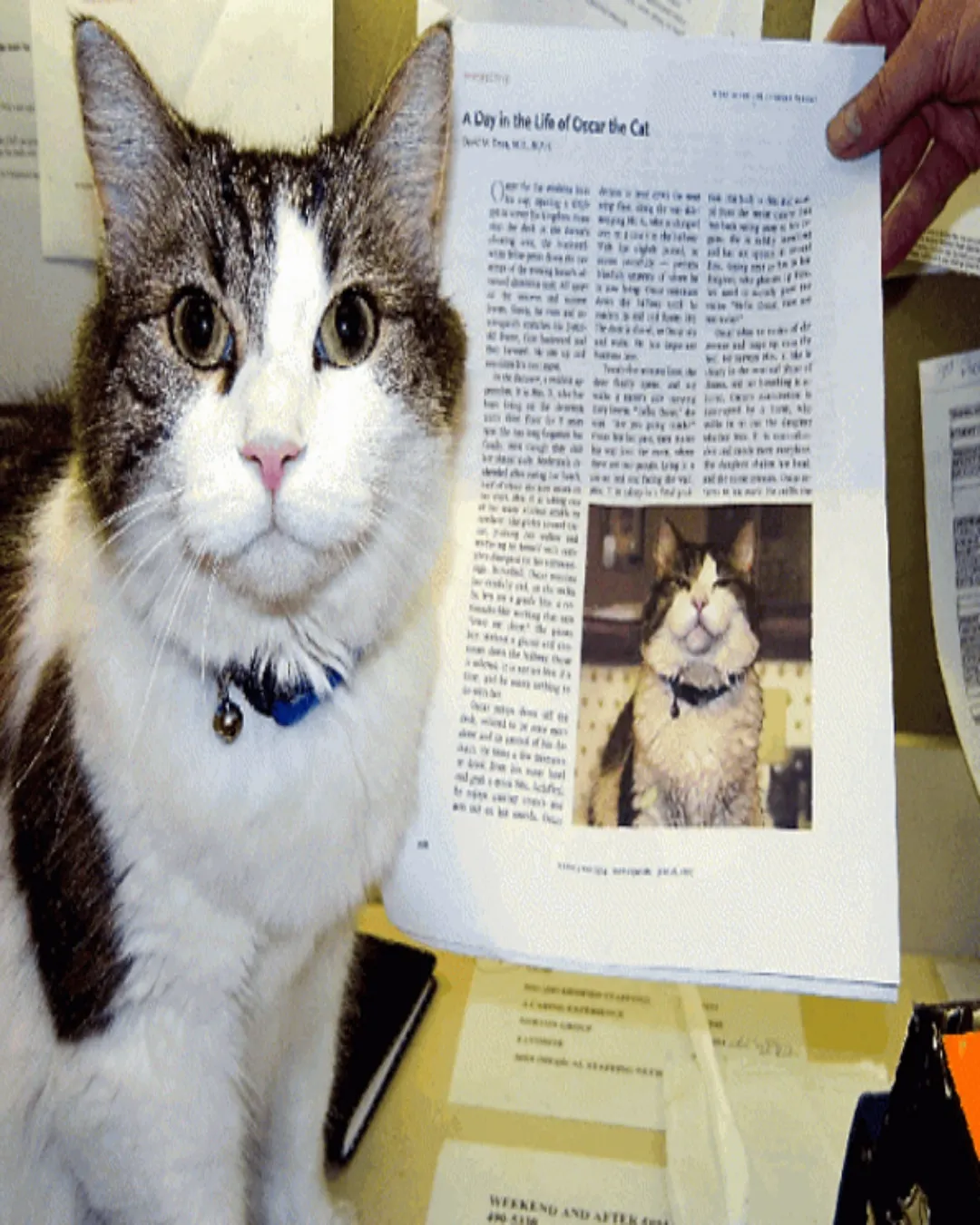
In the animal world, few stories are as mysterious and moving as that of Oscar the cat.
Born in 2005, Oscar was brought to Steere House Nursing and Rehabilitation Center in Rhode Island, USA, where elderly and terminally ill patients spent their final days.
At first glance, Oscar seemed like an ordinary short-haired cat, with piercing green eyes. But soon, nurses and doctors noticed something extraordinary.
Whenever Oscar quietly entered a patient’s room, jumped onto the bed, and curled up beside them, that person would pass away within hours.
At first, staff thought it was coincidence. But as it happened again and again – over 100 times – it was clear that Oscar had a gift.
He could sense death approaching.
Doctors documented that Oscar unfailingly chose the patient whose time had come, even when no medical signs were obvious.
For families, Oscar’s presence became a silent signal. When the cat lay down beside their loved one, they knew the end was near and could gather to say goodbye.
Instead of fear, many felt gratitude. Oscar gave them the chance not to miss those final moments.
One doctor wrote: “Oscar provides something medicine cannot — companionship, warmth, and a peaceful passing.”
In 2007, his story was published in the New England Journal of Medicine, shocking the world. The media called him the “death-predicting cat.”

Scientists offered theories: perhaps Oscar smelled biochemicals released before death, or detected subtle changes in breathing or heart rhythms.
But whatever the explanation, his presence brought comfort and dignity to the dying.
In 2010, the book Making Rounds with Oscar shared the remarkable tale of this compassionate cat.
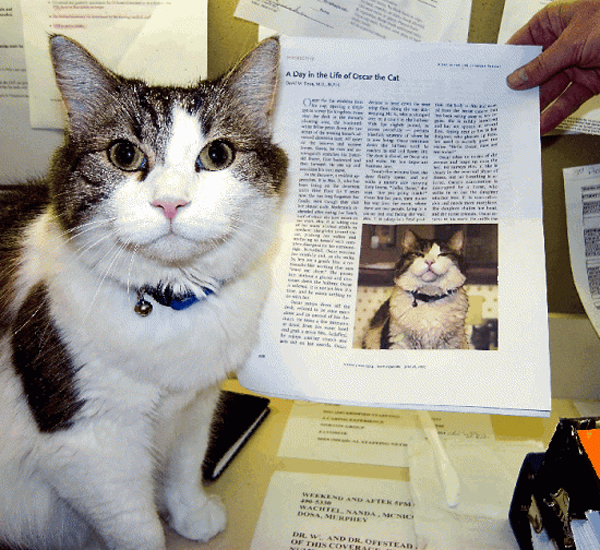
Oscar became a symbol of empathy — not by saving lives, but by making sure no one left the world alone.